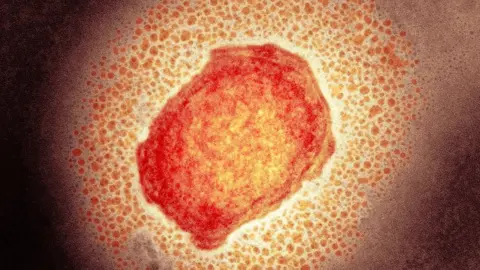
Monkeypox: Doctors concerned over impact on sexual health
 Science Photo Library
Science Photo LibraryMonkeypox could have a "massive impact" on access to sexual health services, doctors have warned.
Staff at clinics are already having to isolate if they have come into contact with anyone infected.
In London, where most of the UK's 20 identified cases have been detected, sexual health clinics have stopped people walking in altogether.
The British Association for Sexual Health and HIV said it was concerned about the effect on other infections.
Cases of monkeypox, which is generally mild, are rare outside Central and West Africa, but about 80 cases have been confirmed in at least 12 countries, the World Health Organization says.
Infections were confirmed in Italy, Sweden, Spain, Portugal, the US and Canada, as well as the UK - where the first European case was reported.
The WHO says another 50 suspected cases are being investigated.
Monkeypox can be spread when someone is in close contact with an infected person. The virus can enter the body through broken skin, or through the eyes, nose or mouth.
It has not previously been described as a sexually transmitted infection, but it can be passed on by direct contact during sex.
And the most recent UK cases are in gay or bisexual men which has prompted the UK Health Security Agency to encourage men who have sex with men to be aware of any unusual rashes or lesions.
They are being asked to contact their local sexual health service if they have concerns.
'Staff have to isolate'
Dr Claire Dewsnap, a consultant in genitourinary medicine and president of the British Association for Sexual Health and HIV, said staff in sexual health clinics were "already under significant pressure" and monkeypox was making that situation worse.
"It is already stretching the workforce and will have a massive impact if staff have to isolate if they are in close contact with someone who's infected," Dr Dewsnap said.
"I am concerned about the potential impact on access to sexual health generally."
In London, clinics are asking all patients to contact staff in advance and tell them their symptoms before being offered an appointment.
This is so those with monkeypox symptoms can be kept away from waiting rooms or clinics where other people are present.
Clinics elsewhere are asking only those with an unusual rash to call ahead so they can be seen in separate areas.
Some staff in sexual health clinics have already received a smallpox vaccine to help protect them against monkeypox - a smallpox jab offers some good protection since the two viruses are quite similar.

What is monkeypox?
 UKHSA
UKHSAMonkeypox is usually associated with travel to Central or West Africa, but some of the cases that have been occurring outside these countries have had no travel link.
It does not spread easily between people, but it can be spread through:
- touching clothing, bedding or towels used by someone with the monkeypox rash
- touching monkeypox skin blisters or scabs
- the coughs or sneezes of a person with the monkeypox rash
If you get infected with monkeypox, it usually takes between five and 21 days for the first symptoms to appear.
Symptoms include fever, headache, muscle aches, backache, swollen lymph nodes, chills and exhaustion.
A rash can develop, often beginning on the face, then spreading to other parts of the body. The rash changes and goes through different stages - a bit like chicken pox - before finally forming a scab, which later falls off.
Read more about the virus here.

Twenty cases of monkeypox have now been confirmed in the UK, with a further 11 announced on Friday, and most have been mild.
However, the disease can be more severe, especially in young children, pregnant women, and people who have weakened immune systems.
Health Secretary Sajid Javid said on Friday that the UK was stocking up on smallpox vaccine doses to help protect some groups against the virus.
A smallpox jab offers some good protection against monkeypox since the two viruses are quite similar.
Ten other countries, including the US, Portugal, Spain and Canada, have also detected cases.
The World Health Organization is convening an emergency meeting with experts about the spread of the virus which is normally found in remote parts of central and west Africa.
Sir Peter Horby, director of the Pandemic Sciences Institute at Oxford University, told BBC Radio 4's Today programme that "it is an unusual situation where we seem to have had the virus introduced but now ongoing transmission within certain communities".
He said that the key message to people with symptoms was to "seek attention, get diagnosed and then to be isolated in some way at home so that they don't spread it on".
Asked how effective current treatments are, he said there was a post-exposure prophylaxis that can be given to close contacts and an anti-viral drug was also being tested in central Africa "so there's a lot that can be done".
